Diseases & Conditions
The Spine: Cervical (Neck) and Lumbar (Back)
Each segment of your spine is crucial to the well being of your entire spine and spinal cord since each part’s strength depends on the other vertebrae and discs to function properly. Constant stress, repetitive or acute injuries and various conditions, such as arthritis, can cause pain.
Pinpointing the source of your pain is key
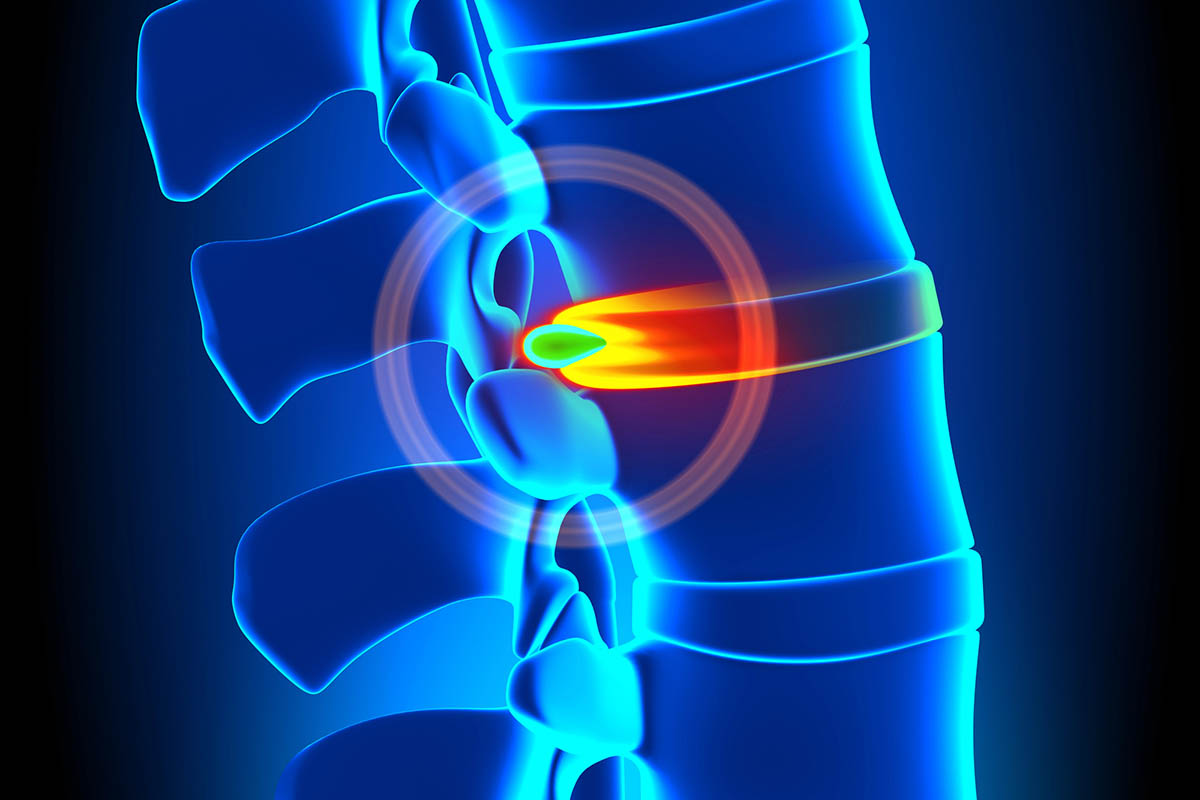
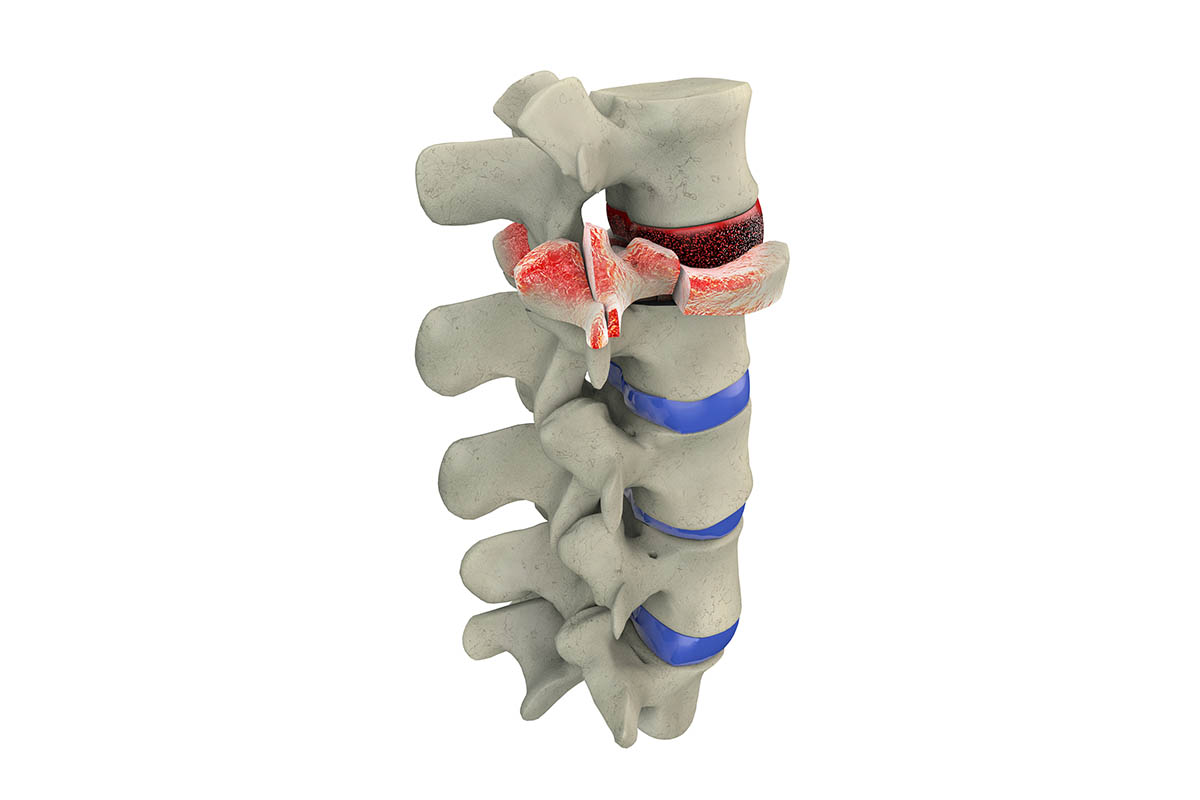
Pinpointing the source of your pain and understanding your problem are the keys to eliminating pain and restoring function. Using the latest technology, our highly trained team of spine and pain management specialists are experts in diagnosing spinal conditions, from a herniated or bulging disc to degenerative disc disease, deformity, spinal stenosis, spondylosis, scoliosis, spondylolisthesis, spinal fractures, infection, spinal tumors and osteoporosis, among others. Learn about these conditions and their symptoms below, based on information from the American Academy of Orthopedic Surgery.

Diseases & Conditions
Degenerative Spine and Disc Conditions
IVD
Intervertebral Disc
Understanding Back & Neck Fractures
Other Conditions of the Spine
Educational Videos
Top 3 things to consider when searching for a spine surgeon - Denver, Colorado
World Renowned Spine Surgeon Dr. Michael Janssen Discusses Motto Around Preparing
Degenerative Spondylolisthesis | Denver Spine Surgeons - Dr. Janssen
Dr Janssen - Denver Spine Surgeon | Colorado Orthopedics | Spinal Stenosis
Dr Janssen | Cervical Disc Replacement - Denver Spine Surgeons
Minimally Invasive Spine Surgery | Dr Janssen - Denver Spine Surgeons
Dr Janssen | Lumbar TDR | Denver Spine Surgeons













CSO Spine & Wine Fall 2024 "Disc Herniations: When do they matter?" Presented by Dr. Jacob Rumley
Center for Spine & Orthopedics October 30, 2024 9:22 pm